Droopy upper eyelid or ptosis presents with substantial blockage of the upper part of field of vision, risk of amblyopia among young children, and an aging change in facial appearance.
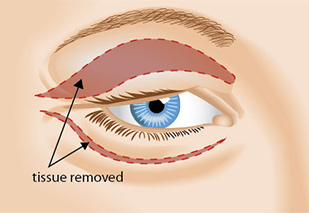
Blepharoptosis is an abnormal low-lying upper eyelid margin with the eye in primary gaze. Normally, the upper lid covers 1.0-2.0mm of the superior part of the cornea. Skin redundancy of the upper lid, or dermatochalasis, is a separate finding, and may occur in conjunction with blepharoptosis. Dermatochalasis should be distinguished from blepharoptosis as the surgical management differs.
Patients usually present with complaint of the involved eye being small, tired appearance, limitation of the field of vision, and headache.
Acquired blepharoptosis can occur at any age, but it is commonly seen in older adults. Congenital blepharoptosis presents from birth. There is no racial or gender predilection in blepharoptosis.
More details are needed in regards to the onset of ptosis, alleviating or aggravating factors, family history of ptosis, recent botulinum injection, and history of trauma or ocular surgery. History usually provides very good clue for the etiology of the blepharoptosis.
It is important to ask about any anticoagulant use or bleeding, a family history of malignant hyperthermia and cardiac disorders such to avoid potential complications during surgery.
Clinical examination is enough in majority of patients. Visual field is usually requested to show the impact of the blepharoptosis peripheral field of vision. In few patients laboratory and imaging studies are needed to find out the cause of the blepharoptosis.
Surgical correction of congenital ptosis can be done at any age depending on the severity of the disease and early intervention is required if there is a risk for development of amblyopia or significant abnormal head position. Different surgical techniques are available for blepharoptosis correction. Depending on treatment goals, the underlying diagnosis, surgeon preference, and the degree of levator function, the appropriate technique is chosen. Patients need to be aware that symmetry is not easy to achieve. Great care should be taken for patients with dry eyes, decrease corneal sensation, absent Bell phenomenon, double elevator palsy, or progressive external ophthalmoplegia to avoid exposure keratopathy postoperatively. If the patient has strabismus and blepharoptosis, strabismus needs to be corrected first.
The surgical correction of blepharoptosis is generally done as an outpatient procedure. While the patient is awake, apply cold compresses to the eyelids for 20 minutes every 1-2 hours for 2-3 days to decrease swelling and bruising. A topical antibiotic ointment (with or without a steroid) is given for the patients to be applied on the eye and the incision site twice daily for 5-7 days. For patients who are expected to have postoperative lagophthalmose, excessive lubrication is needed. Patients usually are seen 1 to 2 weeks following surgery. The patients are evaluated for signs of exposure keratopathy, infection, granuloma formation, and overcorrection and undercorrection. Patients with amblyopia need to continue amblyopia treatment.